Adenomyosis / endometriosis / pelvic pain
So many women have incredibly painful, heavy and debilitating symptoms for the majority of each monthly cycle. Whilst these vary from individual to individual, month to month, and day to day, there are many similarities in the ways our bodies’ respond to pelvic, uterine and ovarian pain and inflammation.
Our nervous systems know what to do to protect us from perceived harm - manifesting as the pain signals that come from inflamed and angry tissues. Our primal response is to ‘lock down’, prevent movement, and hold still as a way to protect us from further insult or injury’. This response is no different to the response to a broken bone - immobilise, reduce blood flow, heighten cortisol, adrenaline and glucose levels. Each of these are great in acute injury, but when what the body perceives as injury happens every day for half, to two thirds or more of every monthly ovulation and menstruation cycle it’s really unhelpful for every-day life and the possibility of healing.
Inflammation is a natural process within the ‘healing’ that happens when endometrial tissues slough away from the uterus, or elsewhere in the pelvis in endometriosis. Inflammatory cycles last around 72 hours in healthy healing and recovery as blood flow is temporarily increased, inflammatory mediators are attracted to the area of ‘injury’, pain producing substances are released to heighten our awareness and take care of the area, nerve endings become sensitive to pressure, heat, cold, and pain substances, and we naturally guard the area by tensing muscles.
All of this happens subconsciously as a result of the autonomic nervous system responses to threat or injury.
When pain signals are really high, fast, or relenting, the process is amplified as a way to protect and repair.
When this happens day after day it’s debilitating, exhausting, impairs sleep quality, affects our ability to exercise, and weakens our immune systems.
Organs need to move
When pain restricts movement and increases muscle tension the natural glide and slide of organs, nerves, fascia, blood vessels, and interstitial fluid is significantly impaired - nowhere more so than the diaphragm, pelvic floor and pelvic-abdominal organs.
If you can imagine tense, inflamed, sensitive nerves being squashed into a tight space - its no wonder we want to double up into a foetal position and pray for it to be over!
The quandry
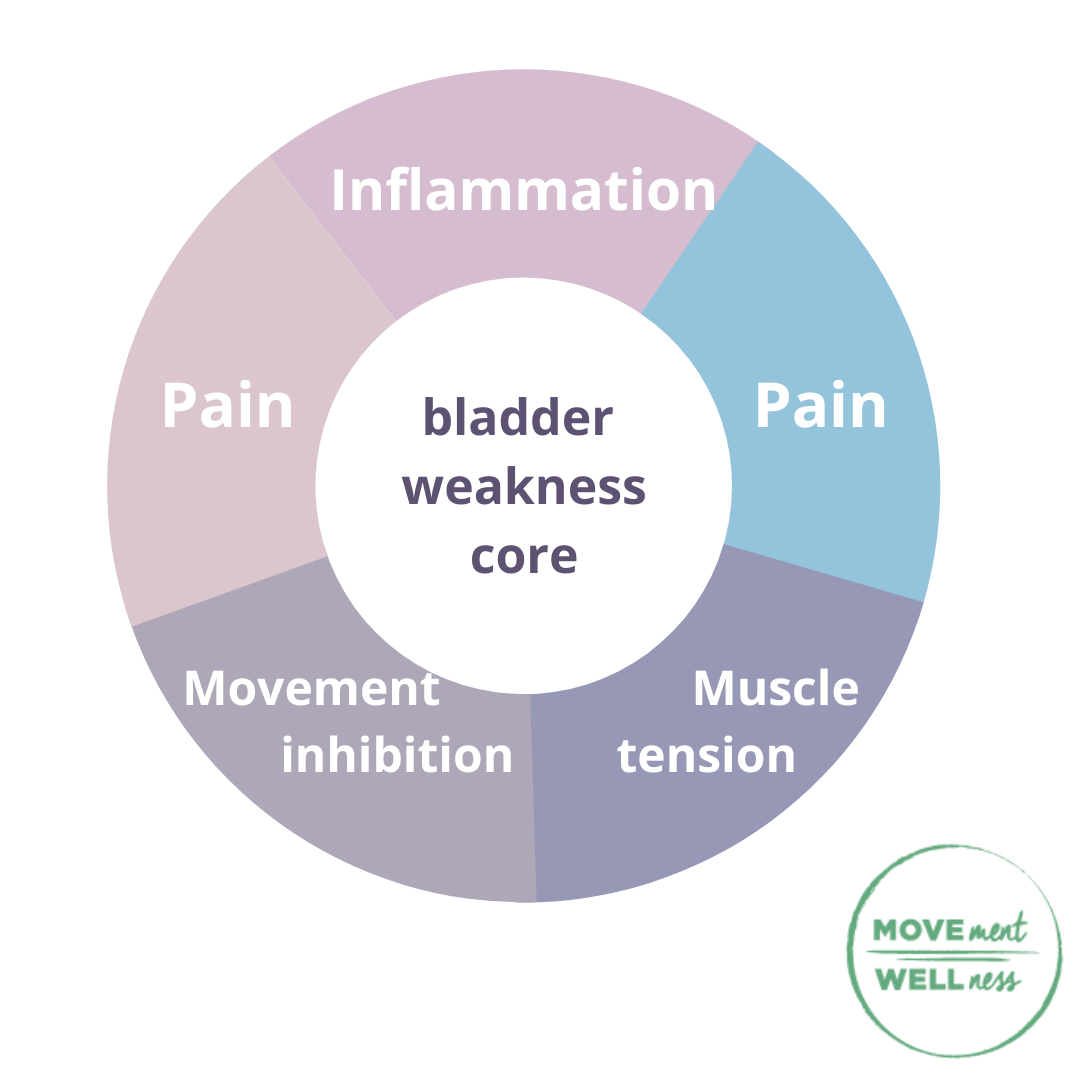
Limited movement creates guarding, stickiness and increased pressure on nerve endings and angry tissues. This increase in pressure can negatively affect bladder function and urination - creating bladder weakness, leakage, urgency, or incomplete emptying of the bladder when we do pass urine.
But the thought of pelvic floor contraction when it hurts is of course challenging, if not impossible to imagine.
Same goes for deep abdominal and back body breathing - how could I do that without making the pain worse.
there is a gentle way
Many kegels-type exercises are too strong, and unnecessary for the level of subtle fascial, organ, muscle, and nerve activation that we need to maintain just enough movement to:
Relieve, rather than increase pain
Cultivate subtle strengthening into the pelvic floor, lower back and diaphragm
Minimise, if not relieve bladder weakness, leakage, and urgency
Yoga therapy can help
Simple
Subtle
Accessible
Breath
Movement
Empowerment
Whether it’s adenomyosis, endometriosis, fibroids, perimenopause, or post surgical recovery - learning to take full, gentle diaphragmatic breaths can open up the possibility to consciously activate pelvic floor and deep abdominal muscles to minimise back pain, pelvic tension, and bladder weakness.